Mild Cognitive Impairment: Overview (Expanded)
Mild Cognitive Impairment (MCI) occupies a critical space in the spectrum of cognitive health, serving as an intermediary stage between the expected cognitive changes of normal aging and the more severe, debilitating decline characteristic of dementia. It’s essential to understand that MCI is not a monolithic condition; rather, it encompasses a diverse range of cognitive presentations, each with its own potential trajectory.
At its core, MCI is defined by cognitive deficits that are noticeable to the individual or those around them, and are objectively measurable through neuropsychological testing, yet do not substantially interfere with the individual’s ability to carry out daily activities. This preservation of functional independence is the key differentiator between MCI and dementia. While someone with MCI might experience increased forgetfulness or difficulty with complex tasks, they can still manage their personal care, household chores, and other routine activities.
MCI is often categorized into two primary subtypes:
- Amnestic MCI:
- This subtype is characterized by prominent memory impairments. Individuals with amnestic MCI may struggle with recalling recent events, learning new information, or remembering appointments.
- Amnestic MCI is often considered a prodromal stage of Alzheimer’s disease, meaning it can be an early indicator of future progression to Alzheimer’s.
- Non-amnestic MCI:
- This subtype involves impairments in cognitive domains other than memory, such as language, executive functions (planning, problem-solving), or visuospatial abilities.
- Non-amnestic MCI can be associated with various underlying pathologies, including vascular disease, frontotemporal dementia, or other neurodegenerative conditions.
The prevalence of MCI increases significantly with age, highlighting the importance of early detection and intervention. As the global population ages, the number of individuals affected by MCI is expected to rise, placing a greater emphasis on understanding its risk factors, diagnosis, and management.
Key aspects of MCI to consider:
- Heterogeneity:
- The diverse presentations of MCI underscore the need for individualized assessment and management.
- Progression:
- While not everyone with MCI progresses to dementia, the risk is elevated, particularly for those with amnestic MCI.
- Quality of life:
- Even though functional independence is preserved, MCI can still impact an individual’s quality of life, leading to anxiety, depression, and reduced self-esteem.
- Research:
- Ongoing research is crucial for identifying biomarkers, developing effective treatments, and improving our understanding of the underlying mechanisms of MCI.
Understanding MCI is vital for healthcare professionals, caregivers, and individuals alike. Early detection, accurate diagnosis, and appropriate management can help mitigate the impact of MCI and improve the lives of those affected.

MCI: Diagnosis (Expanded)
The diagnosis of Mild Cognitive Impairment (MCI) is a multifaceted process that requires a thorough evaluation to distinguish it from normal age-related cognitive changes and other neurological disorders. A comprehensive diagnostic approach typically involves the following key components:
- Detailed Medical History:
- This involves gathering information about the individual’s cognitive complaints, including the onset, duration, and nature of any perceived changes.
- Information from family members or caregivers is crucial, as they may observe subtle cognitive changes that the individual may not recognize.
- The medical history should also include a review of past medical conditions, medications, and lifestyle factors that may contribute to cognitive impairment.
- Neuropsychological Assessment:
- This is a critical component of the diagnostic process, involving standardized tests that evaluate various cognitive domains, including:
- Memory (e.g., immediate and delayed recall, recognition)
- Language (e.g., naming, fluency, comprehension)
- Executive functions (e.g., planning, problem-solving, working memory)
- Attention and processing speed
- Visuospatial abilities (e.g., visual perception, spatial reasoning)
- Commonly used neuropsychological tests include the Montreal Cognitive Assessment (MoCA), the Mini-Mental State Examination (MMSE), and the Clinical Dementia Rating (CDR).
- This is a critical component of the diagnostic process, involving standardized tests that evaluate various cognitive domains, including:
- Neurological Examination:
- This involves a physical examination to assess neurological function, including reflexes, coordination, and sensory function.
- The neurological examination helps rule out other neurological conditions that may cause cognitive impairment, such as stroke, Parkinson’s disease, or multiple sclerosis.
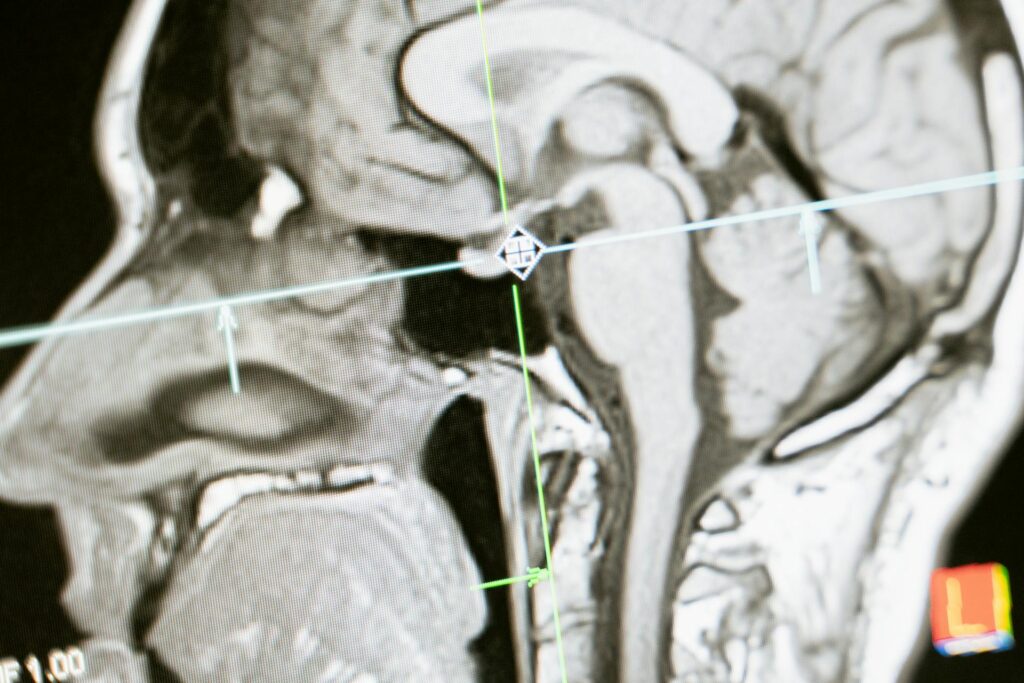
- Brain Imaging:
- Imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT) scans, can provide valuable information about 1 brain structure and function.
- MRI can detect structural changes, such as atrophy, while CT scans can identify vascular lesions or other abnormalities.
- Positron emission tomography (PET) scans can be used to measure brain activity and detect amyloid plaques or tau tangles, which are biomarkers for Alzheimer’s disease.
- Laboratory Tests:
- Blood tests are essential to rule out treatable medical conditions that can cause cognitive impairment, such as:
- Thyroid dysfunction
- Vitamin B12 deficiency
- Electrolyte imbalances
- Infections
- Cerebrospinal fluid (CSF) analysis may be conducted to measure biomarkers of Alzheimer’s disease, such as amyloid-beta and tau proteins.
- Blood tests are essential to rule out treatable medical conditions that can cause cognitive impairment, such as:
- Diagnostic Criteria:
- The diagnosis of MCI typically relies on established diagnostic criteria, such as those developed by the National Institute on Aging and the Alzheimer’s Association.
- These criteria emphasize the presence of objective cognitive impairment, preservation of functional independence, and the absence of dementia.
- Differential Diagnosis:
- It is vital to differentiate MCI from other conditions that can cause cognitive symptoms, such as:
- Depression
- Anxiety
- Sleep disorders
- Medication side effects
- Normal age-related cognitive changes
- It is vital to differentiate MCI from other conditions that can cause cognitive symptoms, such as:
- Follow-up:
- Regular follow-up assessments are crucial to monitor cognitive changes over time and determine if the condition is progressing to dementia.
The careful application of these diagnostic components allows clinicians to accurately identify MCI, determine its subtype, and develop appropriate management strategies.
MCI: Etiology (or MCI: Causes) (Expanded)
The etiology of Mild Cognitive Impairment (MCI) is a complex interplay of various factors, each contributing to the heterogeneous nature of this condition. A deep dive into the causative factors reveals the following key areas:
- Neurodegenerative Processes:
- This is where changes related to diseases like Alzheimers take hold.
- Alzheimer’s Disease Pathology:
- The accumulation of amyloid plaques and neurofibrillary tangles in the brain is a major contributor, particularly in amnestic MCI.
- These pathological changes disrupt neuronal communication and lead to progressive cognitive decline.
- Other neurodegenerative processes, beyond Alzheimers, can also trigger MCI.
- Alzheimer’s Disease Pathology:
- This is where changes related to diseases like Alzheimers take hold.
- Vascular Factors:
- The brains Vascular health plays a vital role.
- Vascular Cognitive Impairment:
- Conditions such as stroke, hypertension, and atherosclerosis impair blood flow to the brain, leading to cognitive deficits.
- Small vessel disease, in particular, can cause subtle but significant cognitive changes.
- Vascular Cognitive Impairment:
- The brains Vascular health plays a vital role.
- Genetic Predisposition:
- Genetics plays a role, with some people having higher predispositions.
- APOE ε4 Allele:
- This genetic variant is a significant risk factor for Alzheimer’s disease and is also associated with an increased risk of MCI.
- Other genetic factors are also being investigated.
- APOE ε4 Allele:
- Genetics plays a role, with some people having higher predispositions.
- Lifestyle Factors:
- Our daily habits impact cognitive health.
- Diet:
- A poor diet, high in saturated fats and processed foods, can increase the risk of cognitive decline.
- Conversely, a diet rich in fruits, vegetables, and omega-3 fatty acids can have protective effects.
- Exercise:
- Regular physical activity has been shown to improve cognitive function and reduce the risk of MCI.
- Social Engagement:
- Maintaining strong social connections and engaging in social activities can also promote cognitive health.
- Diet:
- Our daily habits impact cognitive health.
- Environmental Factors:
- What we are exposed to in our surroundings matters.
- Toxin Exposure:
- Exposure to heavy metals, pesticides, and other toxins can contribute to cognitive decline.
- Air Pollution:
- Studies have linked air pollution to an increased risk of cognitive impairment.
- Toxin Exposure:
- What we are exposed to in our surroundings matters.
- Traumatic Brain Injury (TBI):
- Head injuries can have long term effects on cognition.
- TBI can cause lasting cognitive impairment, including MCI, depending on the severity and location of the injury.
- Head injuries can have long term effects on cognition.
- Chronic Medical Conditions:
- Other health problems can impact the brain.
- Diabetes:
- Diabetes can increase the risk of vascular cognitive impairment.
- Depression:
- Depression can cause cognitive symptoms that mimic MCI.
- Sleep Disorders:
- Sleep apnea and other sleep disorders can impair cognitive function.
- Diabetes:
- Other health problems can impact the brain.
- Inflammatory processes:
- Chronic inflammation in the body is being shown to be a factor in many disease processes, including cognitive decline.
- Hormonal Changes:
- Hormonal changes, especially in women during menopause, may also contribute to cognitive variations.
A thorough understanding of these contributing elements facilitates more accurate risk evaluation, early intervention planning, and the pursuit of more effective prevention methods.
Free consultations. Connect free with local health professionals near you.
Conclusion
Mild Cognitive Impairment (MCI) represents a critical juncture in the continuum of cognitive health, demanding meticulous attention from both healthcare professionals and the broader community. Its significance lies not only in its potential to foreshadow dementia but also in its profound impact on an individual’s quality of life. The journey through MCI is marked by a complex interplay of diagnostic challenges, etiological intricacies, and evolving management strategies.
The diagnostic process, as elucidated, underscores the necessity for a holistic approach, encompassing detailed medical histories, rigorous neuropsychological assessments, and advanced neuroimaging techniques. Differentiating MCI from normal age-related cognitive changes and other neurological conditions requires a nuanced understanding of its diverse presentations and underlying pathologies. This diagnostic rigor is paramount in ensuring accurate identification and timely intervention.
The etiology of MCI, with its multifactorial nature, highlights the interconnectedness of genetic, environmental, and lifestyle factors. From the insidious accumulation of amyloid plaques to the detrimental effects of vascular disease and traumatic brain injury, the causes of MCI are as varied as its manifestations. This complexity necessitates a personalized approach to risk assessment and management, considering each individual’s unique circumstances and vulnerabilities.
Management strategies, while currently focused on mitigating symptoms and slowing progression, are continually evolving. Lifestyle modifications, including regular exercise, a balanced diet, and social engagement, remain cornerstones of care. Cognitive training and the management of comorbid conditions further contribute to maintaining cognitive function and enhancing well-being. The ongoing pursuit of pharmacological interventions and novel therapies holds promise for future advancements in MCI management.
Ultimately, addressing MCI requires a collaborative effort, involving healthcare providers, researchers, caregivers, and individuals themselves. By fostering a deeper understanding of MCI, promoting early detection, and implementing comprehensive management strategies, we can strive to improve the lives of those affected and navigate the complexities of this challenging condition. As research continues to unravel the intricate mechanisms of MCI, we move closer to a future where cognitive decline is better understood, and effective interventions are readily available, offering hope and support to individuals and families facing this cognitive challenge.
Time to feel better. Find a mental, physical health expert that works for you.
Common FAQs:
Mild Cognitive Impairment (MCI)
What is Mild Cognitive Impairment (MCI)?
MCI is a condition where a person experiences cognitive changes, such as memory problems, that are greater than normal age-related changes, but not severe enough to interfere significantly with daily life. 1 It’s considered a transitional stage between normal aging and dementia.
What are the symptoms of MCI?
Symptoms vary, but common ones include:
- Memory problems (especially remembering recent events)
- Difficulty finding words
- Trouble with planning and organizing
- Challenges with visual-spatial tasks
- Slower processing speeds.
Is MCI the same as dementia?
No. MCI is different from dementia. In MCI, cognitive changes are noticeable, but daily functioning is largely preserved. In dementia, cognitive decline significantly impacts daily activities.
Will MCI always lead to dementia?
Not necessarily. Some individuals with MCI remain stable, while others may experience progression to dementia, particularly Alzheimer’s disease. The risk is higher for amnestic MCI (primarily affecting memory).
How is MCI diagnosed?
Diagnosis involves:
- Detailed medical history
- Neuropsychological testing
- Neurological examination
- Brain imaging (MRI, CT)
- Laboratory tests to rule out other causes.
What are the causes of MCI?
Causes are varied and can include:
- Alzheimer’s disease pathology
- Vascular problems (e.g., stroke)
- Genetic factors
- Lifestyle factors (diet, exercise)
- Traumatic brain injury
- Other medical conditions.
Is there a cure for MCI?
Currently, there is no cure. Management focuses on slowing progression and improving quality of life.
What treatments are available for MCI?
Management strategies include:
- Lifestyle modifications (exercise, diet, social engagement)
- Cognitive training
- Management of underlying medical conditions
- Ongoing monitoring.
- Medications are not typically prescribed specifically for MCI, but may be used to treat co-occuring conditions.
Can lifestyle changes help with MCI?
Yes. Healthy lifestyle habits, such as regular exercise, a balanced diet, and social activity, can support cognitive health and may help slow cognitive decline.
What should I do if I suspect I or a loved one has MCI?
Consult a healthcare professional, such as a neurologist or geriatrician, for a comprehensive evaluation. Early diagnosis and intervention are important.
Are there support groups for people with MCI?
Yes. Many organizations provide support groups and resources for individuals with MCI and their families. Checking with local hospitals, and organizations such as the Alzheimer’s Association can provide information on local resources.
What kind of doctor should I see if I am worried about MCI?
A neurologist, geriatrician, or neuropsychologist are the most appropriate medical professionals to assess and diagnose MCI.
NOTICE TO USERS
MindBodyToday is not intended to be a substitute for professional advice, diagnosis, medical treatment, or therapy. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding any mental health symptom or medical condition. Never disregard professional psychological or medical advice nor delay in seeking professional advice or treatment because of something you have read on MindBodyToday.
Share this article

Let us know about your needs so we can answer any of your questions.

Fast and easy to understand quote

We come fully prepared.Hire when ready.
Popular Professionals Near You
You might also like
What is Family Systems Therapy: A…
, What is Family Systems Therapy? Everything you need to know Find a Pro Family Systems Therapy: Understanding the Individual […]
What is Synthesis of Acceptance and…
, What is Dialectical Behavior Therapy (DBT)? Everything you need to know Find a Pro Dialectical Behavior Therapy (DBT): Synthesizing […]
What is Cognitive Behavioral Therapy (CBT)…
, What is Cognitive Behavioral Therapy ? Everything you need to know Find a Pro Cognitive Behavioral Therapy: Theoretical Foundations, […]





