Types and Symptoms
The study of “Types and Symptoms” forms the bedrock of clinical medicine. It’s the process of translating the abstract pathology of a disease into the concrete, lived experience of the patient. This involves not just cataloging symptoms but also understanding their nuances, their progression, and their variability across different populations.
Delving Deeper into Disease Typologies:
Classifying diseases into distinct types is essential for several reasons. First, it allows for a more precise understanding of the underlying mechanisms. For instance, classifying anemia into different types (e.g., iron-deficiency anemia, hemolytic anemia, aplastic anemia) helps pinpoint the specific defect in red blood cell production or destruction. Second, it guides treatment decisions. Different types of a disease often respond to different therapies. For example, the treatment for bacterial pneumonia differs significantly from that for viral pneumonia.
Time to feel better. Find a mental, physical health expert that works for you.
Third, disease classification facilitates research. By grouping patients with similar characteristics, researchers can identify common genetic or environmental factors that contribute to the development of a particular type of disease. Several classification systems are used in medicine, including:
- Etiological classification: This system classifies diseases based on their cause (e.g., infectious diseases, genetic diseases, autoimmune diseases).
- Pathological classification: This system classifies diseases based on the structural or functional abnormalities they produce (e.g., inflammatory diseases, degenerative diseases, neoplastic diseases).
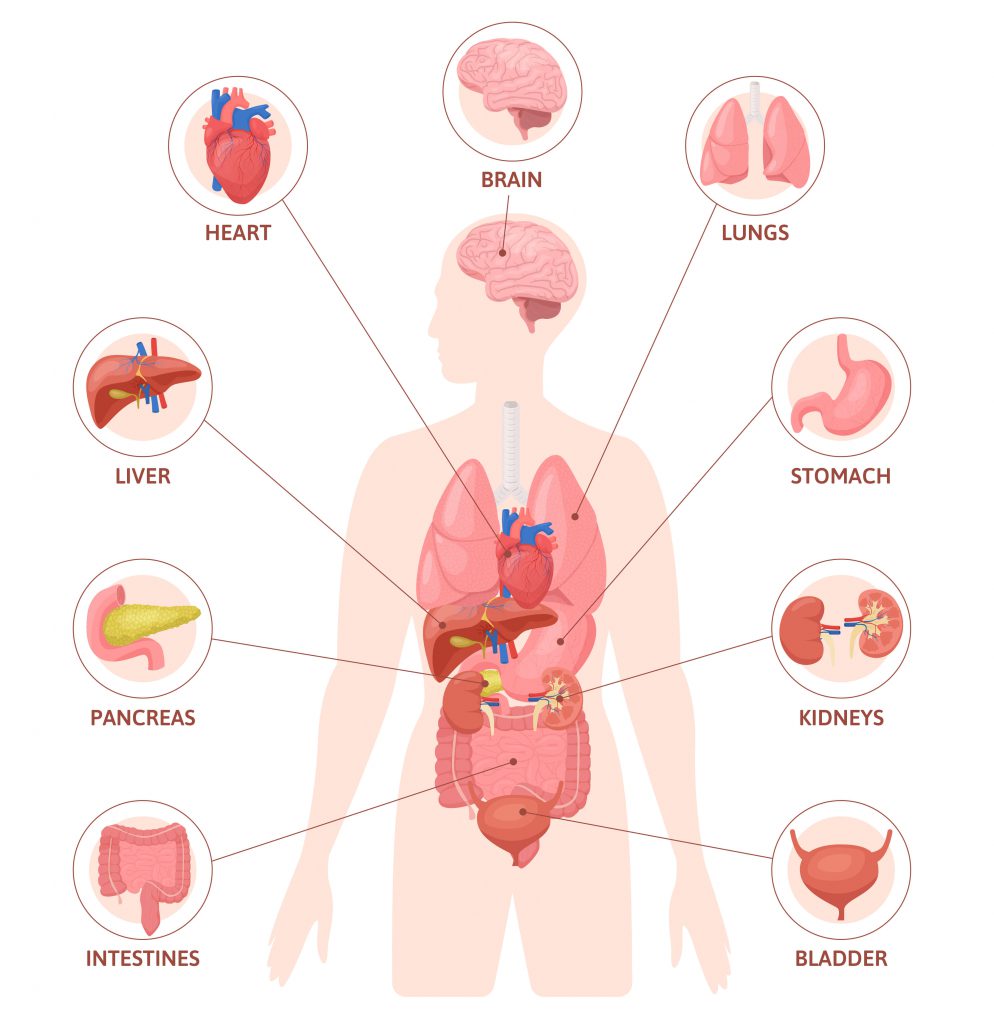
- Clinical classification: This system classifies diseases based on their signs and symptoms (e.g., respiratory diseases, cardiovascular diseases, neurological diseases).
Within each of these broad categories, further subtyping is often necessary. For example, cardiovascular diseases can be subtyped into coronary artery disease, heart failure, arrhythmias, and valvular heart disease, each with its own set of characteristic symptoms and signs.
The Symptom Experience: A Deeper Dive:
Symptoms are the subjective experiences reported by the patient. They are the patient’s perception of their illness and provide valuable clues to the underlying pathology. However, symptoms can be influenced by a variety of factors, including:
- Individual variability: Different people may experience the same disease in different ways. Factors such as age, gender, genetics, and psychological state can all influence symptom perception.
- Cultural factors: Cultural beliefs and norms can shape how people express and interpret their symptoms. In some cultures, for example, it may be more acceptable to express emotional distress through physical symptoms.
- Psychological factors: Anxiety, depression, and stress can all amplify or alter symptom perception. Patients with depression, for example, may report more severe pain or fatigue.
It is crucial for healthcare providers to carefully elicit and interpret symptoms, taking into account these various influencing factors. A detailed symptom history should include the following:
- Onset: When did the symptoms begin? Were they sudden or gradual?
- Location: Where are the symptoms located?
- Intensity: How severe are the symptoms?
- Quality: What do the symptoms feel like? (e.g., sharp, dull, aching, burning)
- Duration: How long do the symptoms last?
- Aggravating and relieving factors: What makes the symptoms worse or better?
- Associated symptoms: Are there any other symptoms present?
Connect Free. Improve your mental and physical health with a professional near you
Objective Signs: The Observable Manifestations:
While symptoms are subjective, signs are objective abnormalities that can be detected by a healthcare provider during a physical examination or through diagnostic tests. Signs provide further evidence of disease and can help to confirm or refute a diagnosis based on symptoms alone. Common signs include:
- Vital sign abnormalities: Fever, tachycardia, bradycardia, hypertension, hypotension, tachypnea, bradypnea
- Physical examination findings: Rashes, swelling, tenderness, abnormal heart sounds, abnormal breath sounds, neurological deficits
- Laboratory abnormalities: Elevated white blood cell count, abnormal electrolyte levels, abnormal liver function tests, abnormal kidney function tests
- Imaging abnormalities: Abnormalities on X-ray, CT scan, MRI, or ultrasound
The interpretation of signs requires clinical expertise and knowledge of the underlying pathophysiology of disease. A particular sign may be associated with multiple different conditions, and healthcare providers must consider the entire clinical picture, including the patient’s symptoms, medical history, and other findings, to arrive at an accurate diagnosis.
Causes and Risk Factors
Understanding the “Causes and Risk Factors” of disease is essential for developing effective prevention strategies and targeted interventions. This involves unraveling the complex interplay of genetic, environmental, and lifestyle factors that contribute to the development of illness.
Genetic Contributions: The Inherited Predisposition:
Genetics plays a significant role in the etiology of many diseases. Inherited genetic mutations can directly cause disease, as in the case of single-gene disorders like cystic fibrosis and Huntington’s disease. In other cases, genetic variations can increase an individual’s susceptibility to developing a disease in response to environmental or lifestyle factors.
Family history is a crucial tool for identifying individuals who may be at increased genetic risk for certain diseases. However, it is important to remember that genetic predisposition does not guarantee that an individual will develop the disease.
Advances in genetic research, such as genome-wide association studies (GWAS), have identified numerous genetic variants associated with common diseases like heart disease, diabetes, and cancer. These findings have improved our understanding of the genetic basis of these diseases and may lead to the development of new diagnostic and therapeutic strategies.
Environmental Influences: The External Exposures:
Environmental factors encompass a wide range of exposures that can contribute to the development of disease. These include:
- Infectious agents: Bacteria, viruses, fungi, and parasites can cause a variety of infectious diseases.
- Chemical exposures: Exposure to toxins, pollutants, and carcinogens in the air, water, and food can increase the risk of various diseases, including cancer and respiratory diseases.
- Radiation: Exposure to ionizing radiation, such as X-rays and gamma rays, can damage DNA and increase the risk of cancer.
- Dietary factors: Unhealthy dietary habits, such as high intake of saturated fat, sugar, and salt, can contribute to the development of obesity, heart disease, diabetes, and other chronic diseases.
The timing and duration of environmental exposures can also be important. Exposure to certain toxins during critical periods of development, such as in utero or early childhood, can have long-lasting effects on health.
Lifestyle Factors: The Behavioral Determinants:
Lifestyle factors play a major role in the development of many chronic diseases. These include:
- Smoking: Smoking is a leading cause of preventable death and is a major risk factor for heart disease, lung cancer, stroke, and other diseases.
- Physical inactivity: Lack of regular physical activity increases the risk of obesity, heart disease, diabetes, and other chronic diseases.
- Excessive alcohol consumption: Excessive alcohol consumption can damage the liver, heart, and brain, and increases the risk of various cancers.
- Unhealthy diet: A diet high in saturated fat, sugar, and salt and low in fruits and vegetables increases the risk of obesity, heart disease, diabetes, and other chronic diseases.
- Stress: Chronic stress can contribute to a variety of health problems, including heart disease, depression, and anxiety.
Lifestyle factors are often modifiable, making them important targets for prevention and intervention. Public health efforts to promote healthy lifestyles can significantly reduce the burden of chronic disease.
Support and Treatment
“Support and Treatment” in medicine encompasses the strategies and interventions aimed at managing disease, alleviating symptoms, and improving the patient’s overall well-being. This involves a multifaceted approach that integrates various modalities, tailored to the individual patient’s needs.
Pharmacological Approaches: The Therapeutic Arsenal:
Pharmacological interventions, or the use of medications, remain a cornerstone of treatment for many diseases. The choice of medication depends on the specific disease, its severity, and the patient’s individual characteristics. Medications can:
- Cure the disease: Antibiotics for bacterial infections, antiviral drugs for viral infections
- Control the disease: Medications for chronic conditions like diabetes, hypertension, and HIV
- Relieve symptoms: Pain medications, anti-nausea medications, anti-depressants
Advances in pharmacology have led to the development of new and more effective medications, including targeted therapies that specifically attack disease-causing molecules. Pharmacogenomics, the study of how genes affect a person’s response to drugs, holds the promise of further personalizing medication therapy.
Non-Pharmacological Interventions: Beyond Medications:
In addition to medications, a variety of non-pharmacological interventions play a crucial role in the management of disease. These include:
- Surgery: Surgical procedures can be used to diagnose, treat, or prevent disease.
- Radiation therapy: Radiation therapy is used to treat cancer by damaging cancer cells.
- Physical therapy: Physical therapy can help patients regain strength, mobility, and function after injury or surgery.
- Occupational therapy: Occupational therapy helps patients adapt to their environment and perform daily activities.
- Speech therapy: Speech therapy helps patients with communication and swallowing disorders.
- Nutritional support: Dietary interventions and nutritional support can be crucial in managing diseases like diabetes, malnutrition, and eating disorders.
- Psychotherapy: Psychotherapy can help patients cope with the emotional and psychological challenges of illness.
Supportive Care: Addressing the Holistic Needs:
Supportive care focuses on improving the patient’s quality of life by addressing their physical, emotional, social, and spiritual needs. This may include:
- Pain management: Strategies to alleviate pain and improve comfort
- Symptom management: Strategies to manage other distressing symptoms like nausea, fatigue, and shortness of breath
- Palliative care: Specialized care for patients with serious illnesses, focused on relieving suffering and improving quality of life
- Psychosocial support: Counseling, support groups, and other resources to help patients and families cope with the emotional and social challenges of illness
- Spiritual care: Addressing the patient’s spiritual needs and concerns
Supportive care is an essential component of comprehensive disease management, particularly for patients with chronic or life-threatening illnesses.
The Importance of a Multidisciplinary Approach
Effective disease management often requires a multidisciplinary approach, involving collaboration among various healthcare professionals, including:
- Physicians
- Nurses
- Pharmacists
- Therapists
- Social workers
- Dieticians
- Psychologists
- Chaplains
This collaborative approach ensures that the patient’s needs are addressed comprehensively and that the treatment plan is coordinated and integrated.

Free consultations. Connect free with local health professionals near you.
Conclusion
In synthesizing the multifaceted aspects of disease, from the initial presentation of “Types and Symptoms” to the intricate exploration of “Causes and Risk Factors,” and finally, the application of “Support and Treatment,” a clear picture emerges of the complexity inherent in medical science. It’s a field that demands not only rigorous scientific inquiry but also a profound understanding of the human experience.
The examination of “Types and Symptoms” underscores the importance of meticulous observation and nuanced interpretation. It highlights how diseases manifest in diverse ways, shaped by individual variability and contextual factors. The subjective nature of symptoms, coupled with the objective reality of signs, necessitates a holistic approach to diagnosis. It reminds us that each patient’s narrative is unique, and that effective healthcare requires empathy and active listening.
Delving into “Causes and Risk Factors” reveals the intricate interplay of genetics, environment, and lifestyle. It illuminates how diseases arise from a complex web of interactions, where inherited predispositions converge with external exposures and behavioral choices. This understanding is crucial for developing preventive strategies and mitigating the burden of illness. It emphasizes the need for public health initiatives that address the social determinants of health and promote healthy lifestyles.
The exploration of “Support and Treatment” underscores the ever-evolving nature of medical interventions. From pharmacological advancements to therapeutic innovations and supportive care, the goal remains to alleviate suffering and enhance quality of life. It highlights the importance of a multidisciplinary approach, where healthcare professionals collaborate to address the holistic needs of patients. And it emphasizes the importance of personalized medicine, where treatment is tailored to the individual’s unique biological profile.
In essence, the study of disease is a continuous journey of discovery, driven by scientific curiosity and a deep commitment to human well-being. 1 As we advance our understanding of disease mechanisms and develop new therapies, we must remain mindful of the individual patient’s experience. Effective healthcare requires a balance of scientific rigor and compassionate care, where the art of medicine complements the science. 2 By embracing this holistic perspective, we can strive to improve health outcomes and enhance the lives of individuals and communities worldwide.
Time to feel better. Find a mental, physical health expert that works for you.
Common FAQs
Regarding Types and Symptoms:
How do doctors determine the different types of a disease?
Can the same symptom indicate different diseases?
Why do some people experience symptoms differently than others with the same condition
What is the difference between a symptom and a sign?
A symptom is a subjective experience reported by the patient (e.g., pain, nausea), while a sign is an objective abnormality that can be detected by a healthcare professional (e.g., fever, rash, abnormal lab results).
When should I be concerned about a symptom and seek medical attention?
Common FAQs
Regarding Causes and Risk Factors:
What are the main types of disease causes?
How do genetic factors influence disease risk?
What are some common environmental risk factors for disease?
How do lifestyle factors contribute to chronic diseases?
Can I prevent diseases by modifying risk factors?
in many cases, yes. Modifying lifestyle factors, such as quitting smoking, adopting a healthy diet, and engaging in regular exercise, can significantly reduce the risk of many chronic diseases.
Common FAQs
Regarding Support and Treatment:
What are the main types of medical treatments?
What is the goal of supportive care?
What is the role of rehabilitation in disease management?
How is treatment tailored to individual patients?
Where can I find support groups for my condition?
People also ask
Q:What is an example of a hallucination?
Q: What causes a person to hallucinate?
A:Hallucinations are caused by the brain misinterpreting sensory input or making incorrect assumptions, leading to the perception of something that isn’t there. Common causes include mental health conditions like schizophrenia, neurological disorders such as dementia or Parkinson’s disease, substance use (drugs or alcohol), sleep deprivation, severe illness, high fevers, and sensory loss. Stress and anxiety can also trigger them. If hallucinations are new, accompanied by detachment from reality, or potentially life-threatening, seek immediate medical evaluation.
Q: How do I know if I'm hallucinating?
Q: What is the first stage of hallucination?
NOTICE TO USERS
MindBodyToday is not intended to be a substitute for professional advice, diagnosis, medical treatment, or therapy. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding any mental health symptom or medical condition. Never disregard professional psychological or medical advice nor delay in seeking professional advice or treatment because of something you have read on MindBodyToday.
Share this article

Let us know about your needs

Quickly reach the right healthcare Pro

Message health care pros and get the help you need.
Popular Healthcare Professionals Near You
You might also like
What is Family Systems Therapy: A…
, What is Family Systems Therapy? Everything you need to know Find a Pro Family Systems Therapy: Understanding the Individual […]
What is Synthesis of Acceptance and…
, What is Dialectical Behavior Therapy (DBT)? Everything you need to know Find a Pro Dialectical Behavior Therapy (DBT): Synthesizing […]
What is Cognitive Behavioral Therapy (CBT)…
, What is Cognitive Behavioral Therapy ? Everything you need to know Find a Pro Cognitive Behavioral Therapy: Theoretical Foundations, […]





