All About Mood Disorders
Understanding Depression
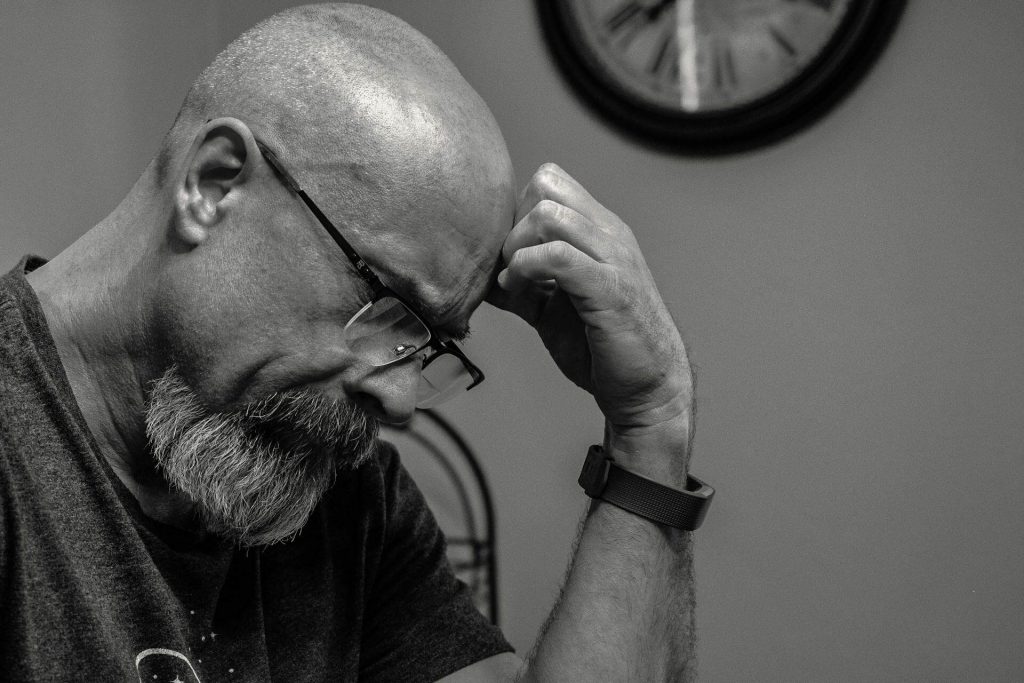
Depression, clinically known as major depressive disorder, is more than just feeling sad. It’s a pervasive and debilitating mental health condition that significantly impacts a person’s thoughts, feelings, and behaviors. Unlike fleeting moments of sadness, depression is characterized by persistent low mood, loss of interest in activities, and a range of physical and cognitive symptoms that interfere with daily life. Understanding depression requires acknowledging its complexity and recognizing it as a legitimate medical condition.
At its core, depression involves a disruption in the brain’s neurochemistry, particularly in the balance
of neurotransmitters like serotonin, dopamine, and norepinephrine. These chemicals play crucial roles in regulating mood, motivation, and pleasure. Genetic predisposition, environmental stressors, and life experiences can all contribute to this chemical imbalance. This biological basis underscores that depression is not a matter of willpower or personal weakness.
The impact of depression extends beyond emotional distress. It can manifest as physical symptoms like fatigue, changes in appetite, sleep disturbances, and unexplained aches and pains. Cognitively, individuals may experience difficulty concentrating, impaired memory, and indecisiveness. Socially, depression can lead to isolation, strained relationships, and withdrawal from previously enjoyed activities.
Understanding depression also involves recognizing its diverse forms. Depression can present as major depressive disorder, persistent depressive disorder (dysthymia), bipolar depression, seasonal affective disorder (SAD), or postpartum depression. Each variant has its own unique characteristics and triggers, requiring tailored approaches to treatment and management.
Furthermore, it is important to destigmatize depression. Misconceptions and societal biases often prevent individuals from seeking help, exacerbating their suffering. Understanding depression means fostering empathy, promoting awareness, and advocating for accessible mental health resources. By acknowledging its biological, psychological, and social dimensions, we can create a more supportive environment for those affected by this challenging condition.
Connect Free. Improve your mental and physical health with a professional near you
Depression Symptoms
Depression manifests through a wide array of symptoms, affecting both mental and physical well-being. These symptoms can vary in intensity and duration, but they consistently disrupt daily functioning. Recognizing these signs is crucial for early intervention and effective management.
A hallmark symptom of depression is persistent sadness or a “low” mood that lingers for most of the day, nearly every day, for at least two weeks. This sadness is often accompanied by a profound loss of interest or pleasure in activities once enjoyed, known as anhedonia. Individuals may withdraw from hobbies, social gatherings, and other sources of joy.
Emotional symptoms extend beyond sadness. Feelings of worthlessness, guilt, and hopelessness are common. Individuals may engage in self-criticism, harbor negative thoughts about themselves and the future, and struggle with excessive or inappropriate guilt. Irritability, frustration, and restlessness are also frequently reported.
Cognitive symptoms include difficulty concentrating, making decisions, and remembering details. Mental fog and slowed thinking can impair performance at work, school, or in everyday tasks. Thoughts of death or suicide, including planning or attempting suicide, are serious warning signs that require immediate attention.
Physical symptoms are equally significant. Changes in appetite, leading to weight loss or gain, are common. Sleep disturbances, such as insomnia or excessive sleep, can further exacerbate fatigue and low energy. Unexplained aches and pains, headaches, and digestive problems can also occur.
Socially, depression can lead to isolation and withdrawal. Individuals may avoid social interactions, neglect relationships, and experience increased conflict with loved ones. This social isolation can perpetuate a cycle of loneliness and worsen depressive symptoms.
It’s important to note that not everyone experiences all these symptoms, and the severity can vary. However, the presence of multiple symptoms, especially persistent sadness or loss of interest, warrants professional evaluation. Early recognition and intervention can significantly improve outcomes and quality of life.
Depression Origins
The origins of depression are multifaceted, involving a complex interplay of biological, psychological, and social factors. No single cause explains every case, and often, a combination of these elements contributes to the development of the disorder.
Biologically, imbalances in brain chemicals, particularly neurotransmitters like serotonin, dopamine, and norepinephrine, play a critical role. These neurotransmitters regulate mood, sleep, appetite, and motivation. Genetic predisposition also increases vulnerability to depression. Individuals with a family history of depression are more likely to develop the condition themselves. Hormonal changes, such as those occurring during puberty, pregnancy, or menopause, can also trigger depressive episodes. Chronic illnesses and certain medications can also contribute to depression.
Psychologically, personality traits like low self-esteem, pessimism, and a tendency to worry can heighten susceptibility. Traumatic life events, such as the loss of a loved one, abuse, or significant stress, can trigger depression. Learned helplessness, a feeling of being unable to control life’s events, can also contribute to depressive symptoms. Cognitive distortions, or negative thinking patterns, perpetuate negative emotions and reinforce depressive thoughts.
Social factors significantly impact depression. Social isolation, lack of social support, and difficult relationships can exacerbate feelings of loneliness and hopelessness. Economic hardship, unemployment, and discrimination can also contribute to stress and depression. Cultural factors and societal stigma surrounding mental health can prevent individuals from seeking help, worsening their condition.
Early childhood experiences, such as abuse, neglect, or exposure to violence, can have long-lasting effects on mental health and increase the risk of depression later in life. These experiences can disrupt the development of healthy coping mechanisms and create a foundation for future mental health challenges.
It is crucial to understand that depression is not a sign of weakness or a personal failing. It arises from a complex interaction of factors, and recognizing this complexity is essential for effective treatment and prevention strategies. A holistic approach that addresses biological, psychological, and social aspects is necessary for comprehensive care.
Depression Treatments
Effective depression treatment typically involves a combination of approaches tailored to the individual’s specific needs and the severity of their condition.
The goal is to alleviate symptoms, restore functionality, and prevent relapse.
Medication:
- Antidepressants are commonly prescribed to regulate brain chemistry. Selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and other types of antidepressants can help stabilize mood, improve sleep, and increase energy levels.
- It’s crucial to work with a healthcare professional to find the right medication and dosage, as individual responses vary. Medication management includes monitoring for side effects and adjusting treatment as needed.
Psychotherapy:
- Talk therapy, or psychotherapy, plays a vital role in depression treatment. Cognitive behavioral therapy (CBT) helps individuals identify and change negative thought patterns and behaviors.
- Interpersonal therapy (IPT) focuses on improving relationship skills and resolving interpersonal conflicts that may contribute to depression.
- Psychodynamic therapy explores how past experiences impact present behaviors.
Electroconvulsive Therapy (ECT):
- In severe cases of treatment-resistant depression, ECT may be considered. This procedure involves delivering controlled electrical pulses to the brain to induce a brief seizure, which can alleviate symptoms.
- ECT is generally safe and effective, but it can cause temporary memory loss.
Lifestyle Changes:
- Adopting healthy lifestyle habits can complement other treatments. Regular exercise, a balanced diet, and sufficient sleep can significantly improve mood and overall well-being.
- Reducing or eliminating alcohol and drug use is also essential, as these substances can exacerbate depressive symptoms.
Combination Therapy:
- Often, the most effective approach involves a combination of medication and psychotherapy. This integrated treatment strategy addresses both the biological and psychological aspects of depression.
- Ongoing monitoring and support are essential for successful depression management.

Free consultations. Connect free with local health professionals near you.
Therapeutic Interventions for Depression
Therapeutic interventions for depression focus on providing individuals with the tools and strategies to manage their symptoms and improve their quality of life.
Cognitive Behavioral Therapy (CBT):
- CBT is a widely used therapy that helps individuals identify and challenge negative thought patterns and distorted beliefs that contribute to depression.
- It teaches coping skills to manage difficult emotions and change behaviors that perpetuate depression.
- CBT is a very structured type of therapy, that focuses on solving current problems.
Interpersonal Therapy (IPT):
- IPT addresses depression by focusing on interpersonal relationships and social functioning.
- It helps individuals identify and resolve relationship problems, such as grief, role transitions, role disputes, and interpersonal deficits.
- IPT aims to improve communication skills and build healthier relationships.
Dialectical Behavior Therapy (DBT):
- DBT, originally developed for borderline personality disorder, can also be effective for depression, particularly when it co-occurs with emotional dysregulation.
- DBT teaches mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness skills.
Psychodynamic Therapy:
- This approach explores unconscious conflicts and past experiences that may contribute to depression.
- It helps individuals gain insight into their emotional patterns and develop healthier coping mechanisms.
Mindfulness-Based Therapies:
- Mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) incorporate mindfulness meditation to increase awareness of thoughts and feelings without judgment.
- These therapies help individuals break free from negative thought cycles and cultivate a greater sense of calm and well-being.
Family Therapy:
- In some cases, family therapy can be beneficial, particularly when depression affects family dynamics.
- It helps family members understand depression, improve communication, and provide support.
Natural Depression Management
While professional treatment is essential for moderate to severe depression, natural approaches can complement therapy and support overall well-being.
Regular Exercise:
- Physical activity releases endorphins, which have mood-boosting effects. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Activities like walking, jogging, swimming, and yoga can be beneficial.
Healthy Diet:
- A balanced diet rich in fruits, vegetables, whole grains, and lean protein can support brain health and improve mood.
- Omega-3 fatty acids, found in fish and flaxseed, have been shown to have antidepressant effects.
- limiting processed foods, and high sugar foods is also very beneficial.
Sufficient Sleep:
- Adequate sleep is crucial for mood regulation. Aim for 7-9 hours of quality sleep each night.
- Establish a regular sleep schedule and create a relaxing bedtime routine.
Sunlight Exposure:
- Sunlight helps regulate serotonin levels. Spend time outdoors each day, especially in the morning.
- If sunlight exposure is limited, consider using a light therapy box.
Stress Management:
- Chronic stress can worsen depression. Practice stress-reduction techniques such as deep breathing, meditation, and yoga.
- Engage in relaxing activities, such as reading, listening to music, or spending time in nature.
Social Support:
- Connecting with friends and family can provide emotional support and reduce feelings of isolation.
- Consider joining a support group to connect with others who are experiencing similar challenges.
Herbal Remedies and Supplements:
- Some herbal remedies, such as St. John’s Wort, and supplements, such as vitamin D, may have mild antidepressant effects. However, it is very important to consult with a doctor before using them, as they can interact with medications.
- These natural remedies should never replace prescribed medical treatments.
Depression Prevention and Coping
Preventing depression and developing effective coping strategies are crucial for maintaining mental well-being. While some individuals may be genetically predisposed, many preventive measures and coping mechanisms can significantly reduce the risk and impact of depressive episodes.
Prevention:
- Building Resilience: Cultivating resilience involves developing the ability to bounce back from adversity. This can be achieved through practicing problem-solving skills, fostering positive self-talk, and building strong social support networks.
- Lifestyle Management: Adopting a healthy lifestyle is fundamental. Regular exercise, a balanced diet, and sufficient sleep are essential for regulating mood and reducing stress. Limiting alcohol and drug use is also vital, as these substances can exacerbate depressive symptoms.
- Stress Reduction: Chronic stress is a significant risk factor for depression. Techniques like mindfulness, meditation, yoga, and deep breathing exercises can effectively manage stress levels.
- Social Connection: Maintaining strong social connections is crucial for emotional well-being. Engaging in social activities, nurturing relationships, and seeking support from friends and family can provide a buffer against depression.
- Early Intervention: Recognizing early warning signs of depression, such as persistent sadness, loss of interest, or changes in sleep and appetite, and seeking professional help promptly can prevent the condition from worsening.
- Cognitive Restructuring: Learning to identify and challenge negative thought patterns can prevent the development of depressive thinking. Cognitive behavioral therapy (CBT) techniques can be helpful in this regard.
Coping:
- Developing Coping Skills: Identifying healthy coping mechanisms is essential for managing depressive symptoms. This may include engaging in hobbies, practicing relaxation techniques, or seeking social support.
- Maintaining Routine: Establishing a daily routine can provide structure and a sense of control, which can be particularly helpful during depressive episodes.
- Self-Care: Prioritizing self-care activities, such as taking baths, reading, or listening to music, can promote relaxation and reduce stress.
- Mindfulness and Acceptance: Practicing mindfulness can help individuals stay present and accept their emotions without judgment. This can reduce the tendency to ruminate on negative thoughts.
- Setting Realistic Goals: Breaking down tasks into smaller, manageable steps can prevent feelings of overwhelm and promote a sense of accomplishment.
- Seeking Professional Help: When coping strategies are insufficient, seeking professional help from a therapist or psychiatrist is essential.
The Neurobiology of Depression
The neurobiology of depression involves intricate interactions within the brain, affecting neurotransmitters, brain structures, and hormonal systems. Understanding these biological underpinnings is crucial for developing effective treatments.
Neurotransmitter Imbalances: Depression is often associated with imbalances in neurotransmitters, particularly serotonin, norepinephrine, and dopamine. These chemicals play key roles in regulating mood, motivation, and pleasure.
- Serotonin is involved in mood regulation, sleep, and appetite.
- Norepinephrine affects alertness, energy, and attention.
- Dopamine influences motivation, pleasure, and reward.
Brain Structure and Function: Studies have shown that certain brain regions are affected in depression.
- The hippocampus, involved in memory and emotion regulation, may be smaller in individuals with chronic depression.
- The prefrontal cortex, responsible for decision-making and emotional control, may exhibit reduced activity.
- The amygdala, which processes emotions like fear and sadness, may be overactive.
Hormonal Influences: Hormones play a significant role in depression.
- The hypothalamic-pituitary-adrenal (HPA) axis, which regulates the stress response, may be overactive, leading to increased cortisol levels.
- Thyroid hormones, which affect metabolism and mood, can also contribute to depressive symptoms.
- Fluctuations in estrogen and progesterone can contribute to depression, especially in women.
Neuroplasticity: Depression can affect neuroplasticity, the brain’s ability to reorganize itself by forming new neural connections. Chronic stress and depression can impair neuroplasticity, making it harder for the brain to recover.
Genetic Factors: Genetic predisposition plays a role in depression. Variations in genes related to neurotransmitter function, stress response, and brain structure can increase vulnerability.
Inflammatory Processes: Recent research suggests that inflammation may contribute to depression. Elevated levels of inflammatory markers in the brain can disrupt neurotransmitter function and contribute to depressive symptoms.
Depression Variants
Depression manifests in various forms, each with unique characteristics and diagnostic criteria. Recognizing these variants is essential for providing tailored treatment and support.
Major Depressive Disorder (MDD):
- Characterized by persistent sadness, loss of interest, and other symptoms that interfere with daily life.
- Symptoms must be present for at least two weeks.
- Can occur as a single episode or recurrent episodes.
Persistent Depressive Disorder (Dysthymia):
- A chronic form of depression with milder symptoms that last for at least two years.
- Individuals may experience persistent low mood, fatigue, and low self-esteem.
- Can be more challenging to diagnose due to its chronic nature.
Bipolar Depression:
- Occurs as part of bipolar disorder, which involves alternating periods of depression and mania or hypomania.
- Depressive episodes can be severe and require careful management.
- Treatment involves mood stabilizers and other medications.
Seasonal Affective Disorder (SAD):
- A type of depression that occurs during specific seasons, typically in the fall or winter, when there is less sunlight.
- Symptoms include fatigue, low energy, and increased appetite.
- Light therapy is often an effective treatment.
Postpartum Depression:
- Occurs after childbirth and involves intense sadness, anxiety, and fatigue.
- Can interfere with bonding with the baby and require immediate treatment.
- Hormonal changes and stress contribute.
Premenstrual Dysphoric Disorder (PMDD):
- A severe form of premenstrual syndrome (PMS) that causes significant emotional and physical symptoms in the week or two before menstruation.
- Symptoms include irritability, depression, and anxiety.
- Treatment may involve medication and lifestyle changes.
Atypical Depression:
- Characterized by increased appetite, excessive sleep, and sensitivity to rejection.
- Individuals may experience improved mood in response to positive events.
- Responds well to certain antidepressants.
1. Depression Prevention and Coping
Preventing depression and developing effective coping strategies are crucial for maintaining mental well-being. While some individuals may be genetically predisposed, many preventive measures and coping mechanisms can significantly reduce the risk and impact of depressive episodes.
Prevention:
- Building Resilience: Cultivating resilience involves developing the ability to bounce back from adversity. This can be achieved through practicing problem-solving skills, fostering positive self-talk, and building strong social support networks.
- Lifestyle Management: Adopting a healthy lifestyle is fundamental. Regular exercise, a balanced diet, and sufficient sleep are essential for regulating mood and reducing stress. Limiting alcohol and drug use is also vital, as these substances can exacerbate depressive symptoms.
- Stress Reduction: Chronic stress is a significant risk factor for depression. Techniques like mindfulness, meditation, yoga, and deep breathing exercises can effectively manage stress levels.
- Social Connection: Maintaining strong social connections is crucial for emotional well-being. Engaging in social activities, nurturing relationships, and seeking support from friends and family can provide a buffer against depression.
- Early Intervention: Recognizing early warning signs of depression, such as persistent sadness, loss of interest, or changes in sleep and appetite, and seeking professional help promptly can prevent the condition from worsening.
- Cognitive Restructuring: Learning to identify and challenge negative thought patterns can prevent the development of depressive thinking. Cognitive behavioral therapy (CBT) techniques can be helpful in this regard.
Coping:
- Developing Coping Skills: Identifying healthy coping mechanisms is essential for managing depressive symptoms. This may include engaging in hobbies, practicing relaxation techniques, or seeking social support.
- Maintaining Routine: Establishing a daily routine can provide structure and a sense of control, which can be particularly helpful during depressive episodes.
- Self-Care: Prioritizing self-care activities, such as taking baths, reading, or listening to music, can promote relaxation and reduce stress.
- Mindfulness and Acceptance: Practicing mindfulness can help individuals stay present and accept their emotions without judgment. This can reduce the tendency to ruminate on negative thoughts.
- Setting Realistic Goals: Breaking down tasks into smaller, manageable steps can prevent feelings of overwhelm and promote a sense of accomplishment.
- Seeking Professional Help: When coping strategies are insufficient, seeking professional help from a therapist or psychiatrist is essential.
2. The Neurobiology of Depression
The neurobiology of depression involves intricate interactions within the brain, affecting neurotransmitters, brain structures, and hormonal systems. Understanding these biological underpinnings is crucial for developing effective treatments.
Neurotransmitter Imbalances: Depression is often associated with imbalances in neurotransmitters, particularly serotonin, norepinephrine, and dopamine. These chemicals play key roles in regulating mood, motivation, and pleasure.
- Serotonin is involved in mood regulation, sleep, and appetite.
- Norepinephrine affects alertness, energy, and attention.
- Dopamine influences motivation, pleasure, and reward.
Brain Structure and Function: Studies have shown that certain brain regions are affected in depression.
- The hippocampus, involved in memory and emotion regulation, may be smaller in individuals with chronic depression.
- The prefrontal cortex, responsible for decision-making and emotional control, may exhibit reduced activity.
- The amygdala, which processes emotions like fear and sadness, may be overactive.
Hormonal Influences: Hormones play a significant role in depression.
- The hypothalamic-pituitary-adrenal (HPA) axis, which regulates the stress response, may be overactive, leading to increased cortisol levels.
- Thyroid hormones, which affect metabolism and mood, can also contribute to depressive symptoms.
- Fluctuations in estrogen and progesterone can contribute to depression, especially in women.
Neuroplasticity: Depression can affect neuroplasticity, the brain’s ability to reorganize itself by forming new neural connections. Chronic stress and depression can impair neuroplasticity, making it harder for the brain to recover.
Genetic Factors: Genetic predisposition plays a role in depression. Variations in genes related to neurotransmitter function, stress response, and brain structure can increase vulnerability.
Inflammatory Processes: Recent research suggests that inflammation may contribute to depression. Elevated levels of inflammatory markers in the brain can disrupt neurotransmitter function and contribute to depressive symptoms.
3. Depression Variants
Depression manifests in various forms, each with unique characteristics and diagnostic criteria. Recognizing these variants is essential for providing tailored treatment and support.
Major Depressive Disorder (MDD):
- Characterized by persistent sadness, loss of interest, and other symptoms that interfere with daily life.
- Symptoms must be present for at least two weeks.
- Can occur as a single episode or recurrent episodes.
Persistent Depressive Disorder (Dysthymia):
- A chronic form of depression with milder symptoms that last for at least two years.
- Individuals may experience persistent low mood, fatigue, and low self-esteem.
- Can be more challenging to diagnose due to its chronic nature.
Bipolar Depression:
- Occurs as part of bipolar disorder, which involves alternating periods of depression and mania or hypomania.
- Depressive episodes can be severe and require careful management.
- Treatment involves mood stabilizers and other medications.
Seasonal Affective Disorder (SAD):
- A type of depression that occurs during specific seasons, typically in the fall or winter, when there is less sunlight.
- Symptoms include fatigue, low energy, and increased appetite.
- Light therapy is often an effective treatment.
Postpartum Depression:
- Occurs after childbirth and involves intense sadness, anxiety, and fatigue.
- Can interfere with bonding with the baby and require immediate treatment.
- Hormonal changes and stress contribute.
Premenstrual Dysphoric Disorder (PMDD):
- A severe form of premenstrual syndrome (PMS) that causes significant emotional and physical symptoms in the week or two before menstruation.
- Symptoms include irritability, depression, and anxiety.
- Treatment may involve medication and lifestyle changes.
Atypical Depression:
- Characterized by increased appetite, excessive sleep, and sensitivity to rejection.
- Individuals may experience improved mood in response to positive events.
- Responds well to certain antidepressants.
Depression and Physical Comorbidities
Depression often coexists with various physical health conditions, creating a complex interplay that can significantly impact overall well-being. These comorbid conditions can exacerbate depressive symptoms and make treatment more challenging. Understanding these connections is crucial for comprehensive care.
Cardiovascular Disease:
- Depression is a significant risk factor for cardiovascular disease. Individuals with depression are more likely to develop heart disease, and those with heart disease are more prone to depression.
- Shared risk factors, such as chronic stress, inflammation, and unhealthy lifestyle habits, contribute to this association.
- Depression can also make it harder for individuals to adhere to cardiac rehabilitation and medication regimens.
Diabetes:
- Depression is twice as common in people with diabetes compared to the general population.
- The stress of managing a chronic illness like diabetes can contribute to depression. Conversely, depression can make it harder to manage blood sugar levels and adhere to treatment plans.
- This bidirectional relationship requires integrated care that addresses both mental and physical health.
Chronic Pain:
- Chronic pain and depression often coexist. Pain can lead to depression, and depression can intensify pain perception.
- The shared neural pathways and neurotransmitter systems involved in pain and mood regulation contribute to this overlap.
- Treating both conditions simultaneously is essential for improving quality of life.
Thyroid Disorders:
- Hypothyroidism, or an underactive thyroid, can mimic or exacerbate depressive symptoms, such as fatigue, low mood, and cognitive difficulties.
- Routine thyroid testing can be necessary when assessing for depression.
- Treating thyroid disorders can improve both physical and mental health.
Obesity:
- Obesity and depression share a complex relationship. Depression can lead to unhealthy eating habits and reduced physical activity, contributing to weight gain.
- Conversely, the stigma and physical limitations associated with obesity can contribute to depression.
- Lifestyle interventions and psychological support are essential for managing both conditions.
Neurological Conditions:
- Conditions like Parkinson’s disease, multiple sclerosis, and stroke often involve depression as a comorbid condition.
- Neurological changes in the brain can directly contribute to mood disturbances.
- Integrated care that addresses neurological and psychological symptoms is vital.
Depression and Suicidality
Depression is a significant risk factor for suicidal thoughts and behaviors. Understanding the link between depression and suicidality is crucial for prevention and intervention.
Risk Factors:
- Severe depression, particularly when untreated, increases the risk of suicide.
- Feelings of hopelessness, worthlessness, and unbearable emotional pain are strong predictors of suicidal ideation.
- Co-occurring mental health conditions, such as anxiety disorders or substance abuse, further increase the risk.
- Past suicide attempts, family history of suicide, and access to lethal means are also significant risk factors.
Warning Signs:
- Increased talk about death or suicide.
- Expressions of hopelessness or feeling trapped.
- Withdrawal from social activities and loved ones.
- Giving away possessions or saying goodbye.
- Sudden mood improvement after a period of deep depression.
- Increased use of alcohol or drugs.
Intervention:
- If someone expresses suicidal thoughts, it is crucial to take them seriously and seek immediate professional help.
- Do not leave the person alone.
- Remove any potentially dangerous objects, such as firearms or medications.
- Contact a crisis hotline or mental health professional.
- Hospitalization may be necessary in severe cases.
Prevention:
- Effective treatment of depression, including medication and therapy, is essential for reducing suicide risk.
- Building strong social support networks can provide a buffer against suicidal thoughts.
- Promoting mental health awareness and reducing stigma can encourage individuals to seek help.
- Access to crisis hotlines and mental health resources is crucial for timely intervention.
Post-vention:
- When a suicide occurs, providing support to family and friends is essential.
- Grief counseling and support groups can help individuals cope with the loss.
- Understanding the factors that contributed to the suicide can inform prevention efforts.
Pediatric Depression
Depression in children and adolescents is a serious mental health condition that requires careful attention and intervention. It can significantly impact their academic performance, social development, and overall well-being.
Prevalence and Characteristics:
- Pediatric depression is more common than many people realize, affecting a significant percentage of children and adolescents.
- Symptoms can differ from those in adults. Children may exhibit irritability, anger, and behavioral problems more than sadness.
- Academic difficulties, social withdrawal, and physical complaints are also common.
Risk Factors:
- Family history of depression, exposure to trauma or abuse, and stressful life events can increase the risk.
- Learning disabilities, chronic illnesses, and social isolation can also contribute.
- Genetic and biological factors play a role.
Diagnosis:
- Diagnosing pediatric depression requires a comprehensive evaluation by a mental health professional.
- Clinicians will assess symptoms, developmental history, and family background.
- It is crucial to differentiate depression from normal developmental changes and other mental health conditions.
Treatment:
- Treatment typically involves a combination of therapy and medication.
- Cognitive behavioral therapy (CBT) and interpersonal therapy (IPT) can help children develop coping skills and manage emotions.
- Antidepressant medications, such as SSRIs, may be prescribed for moderate to severe depression.
- Family involvement is crucial for successful treatment.
Prevention and Early Intervention:
- Promoting positive mental health in schools and communities can help prevent depression.
- Early identification and intervention are essential for preventing the condition from worsening.
- Educating parents, teachers, and healthcare providers about the signs and symptoms of pediatric depression is crucial.
- Creation of supportive school environments, and promotion of social emotional learning in young people is also very helpful.
Conclusion
Depression, in its myriad forms, represents a profound and pervasive challenge to individuals, families, and society as a whole. From the intricate neurobiological underpinnings to the complex interplay of psychological and social factors, it is clear that depression is not a singular entity but a multifaceted condition requiring a holistic approach. The articles presented have illuminated the diverse facets of this disorder, underscoring the necessity for a nuanced understanding that transcends simplistic explanations.
The importance of recognizing the varied symptoms, from persistent sadness and anhedonia to physical manifestations like fatigue and sleep disturbances, cannot be overstated. Early identification is crucial for timely intervention, preventing the escalation of symptoms and the development of comorbid conditions. Furthermore, the exploration of depression’s origins highlights the significance of addressing both biological vulnerabilities and environmental stressors. Genetic predispositions, neurotransmitter imbalances, and hormonal fluctuations interact with life experiences, trauma, and social determinants to shape an individual’s susceptibility.
Treatment strategies, encompassing medication, psychotherapy, and lifestyle modifications, offer hope and pathways to recovery. Cognitive behavioral therapy, interpersonal therapy, and mindfulness-based interventions provide individuals with essential tools to manage their emotions and challenge negative thought patterns. Natural approaches, such as exercise, healthy diet, and stress reduction techniques, complement these therapies, fostering overall well-being.
Prevention and coping mechanisms are equally vital. Building resilience, fostering social connections, and practicing self-care can mitigate the impact of depressive episodes. The recognition of depression variants, including major depressive disorder, bipolar depression, and seasonal affective disorder, underscores the need for tailored interventions that address specific symptom profiles and underlying causes.
The co-occurrence of depression with physical comorbidities, such as cardiovascular disease and diabetes, highlights the importance of integrated care that addresses both mental and physical health. The profound link between depression and suicidality necessitates urgent attention and intervention, emphasizing the need for crisis support and prevention strategies. Finally, the prevalence of pediatric depression calls for a concerted effort to promote mental health awareness and provide timely support to children and adolescents.
In conclusion, the enduring challenge of depression demands a comprehensive and compassionate response. By fostering understanding, promoting early intervention, and advocating for accessible mental health resources, we can create a society that supports individuals in their journey towards recovery and resilience. It is a shared responsibility to destigmatize mental illness, promote empathy, and ensure that those affected by depression receive the care and support they deserve.
Time to feel better. Find a mental, physical health expert that works for you.
Common FAQs:
General Understanding:
What's the difference between sadness and depression?
Sadness is a normal emotion, usually triggered by a specific event and temporary. Depression is a persistent state of low mood, loss of interest, and other symptoms that interfere with daily life, lasting for weeks or months.
Is depression a sign of weakness?
No. Depression is a medical condition, not a personal failing. It’s caused by a combination of biological, psychological, and social factors.
Can depression be cured?
While there’s no single “cure,” depression is highly treatable. With appropriate treatment, many people experience significant improvement and go on to live fulfilling lives.
Can stress cause depression?
Yes, chronic stress can significantly increase the risk of developing depression.
Symptoms and Causes:
What are the main symptoms of depression?
Common symptoms include persistent sadness, loss of interest, changes in appetite and sleep, fatigue, feelings of worthlessness, difficulty concentrating, and thoughts of death or suicide.
What causes depression?
Depression is caused by a complex interplay of factors, including genetic predisposition, brain chemistry imbalances, stressful life events, and psychological vulnerabilities.
Can physical health problems cause depression?
Yes, certain medical conditions, such as thyroid disorders, chronic pain, and heart disease, can contribute to depression.
Treatment and Coping:
What are the most common treatments for depression?
Common treatments include medication (antidepressants), psychotherapy (talk therapy), and lifestyle changes.
Can therapy alone treat depression?
Yes, for mild to moderate depression, therapy can be very effective. For severe depression, a combination of therapy and medication is often recommended.
What are some natural ways to manage depression?
Natural approaches include regular exercise, a healthy diet, sufficient sleep, stress management techniques, and social support.
How can I help someone who is depressed?
Offer support and understanding, encourage them to seek professional help, and avoid minimizing their feelings.
When should I seek professional help for depression?
If you’re experiencing persistent symptoms that interfere with your daily life, or if you’re having thoughts of self-harm 1 or suicide, seek professional help immediately.
Are there support groups for people with depression?
Yes, many support groups, both in-person and online, can provide valuable support and connection.
Is there a test for depression?
There is no blood test, or physical test for depression. Diagnosis is made through clinical interview, and standardized questionaires.
NOTICE TO USERS
MindBodyToday is not intended to be a substitute for professional advice, diagnosis, medical treatment, or therapy. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding any mental health symptom or medical condition. Never disregard professional psychological or medical advice nor delay in seeking professional advice or treatment because of something you have read on MindBodyToday.
Share this article

Let us know about your needs so we can answer any of your questions.

Fast and easy to understand quote

We come fully prepared.Hire when ready.
Popular Professionals Near You
You might also like
What is Family Systems Therapy: A…
, What is Family Systems Therapy? Everything you need to know Find a Pro Family Systems Therapy: Understanding the Individual […]
What is Synthesis of Acceptance and…
, What is Dialectical Behavior Therapy (DBT)? Everything you need to know Find a Pro Dialectical Behavior Therapy (DBT): Synthesizing […]
What is Cognitive Behavioral Therapy (CBT)…
, What is Cognitive Behavioral Therapy ? Everything you need to know Find a Pro Cognitive Behavioral Therapy: Theoretical Foundations, […]





